Asacol is a brand of mesalamine delayed release tablets, a 5-aminosalicylic acid (5-ASA) drug used primarily to treat chronic inflammatory bowel disease, including ulcerative colitis.
It is designed to release mesalamine in the intestine, where it acts locally to reduce inflammation in the lining of the colon, and many patients are kept on the medication for years to control flares, stomach pain, and other symptoms of inflammatory bowel disease.
Asacol (mesalamine) is not a general pain or arthritis medication.
It is a bowel-targeted anti-inflammatory most often prescribed for ulcerative colitis and other inflammatory bowel diseases.
Some confusion comes from sulfasalazine, a related drug that is used in arthritis, but the risks discussed on this page involve mesalamine as a treatment for inflammatory bowel disease, not routine pain control.
Because Asacol is often prescribed for long-term management, patients treated with this drug may accumulate a significant cumulative exposure over time, which increases the importance of careful renal function monitoring throughout treatment.
From the drug’s earliest labeling, the FDA and manufacturer have warned that Asacol and related mesalamine delayed release tablets can injure the kidneys.
The Asacol prescribing information states that “renal impairment, including minimal change disease, acute and chronic interstitial nephritis, and renal failure, has been reported in patients taking products such as Asacol that contain mesalamine or are converted to mesalamine,” and directs prescribers to evaluate renal function before starting therapy and periodically during treatment.
In other words, the label itself recognizes that serious adverse reactions involving the kidneys are a known risk, and that frequent monitoring is part of safe prescribing.
Scientific literature and post-marketing safety data reinforce this connection between mesalamine and renal disease.
Reviews and cohort studies describe an idiosyncratic pattern of renal involvement in patients treated with 5-ASA drugs, most often in the form of tubulointerstitial injury such as acute or chronic interstitial nephritis, and sometimes progressing to chronic kidney disease or end-stage renal disease.
This injury can develop even in people who start with normal kidney function and have no prior history of renal disease.
Multiple peer-reviewed studies, case series, and regulatory documents describe the kidney risks associated with Asacol and other mesalamine products:
- FDA / DailyMed labeling – mesalamine delayed release tablets: Package inserts for mesalamine delayed release tablets, including Asacol and similar products, state that renal impairment (including minimal change nephropathy, acute and chronic interstitial nephritis, and renal failure) has been reported in patients treated with these drugs. The labeling instructs clinicians to assess renal function at the start of therapy and periodically during treatment, and to discontinue the medication if renal function deteriorates.
- The Association of Mesalamine With Kidney Disease – (Advances in Chronic Kidney Disease): This review summarizes suspected adverse reaction reports and clinical data linking mesalamine to adverse kidney effects, including chronic interstitial nephritis and chronic kidney disease. It notes that product labels consistently warn of renal impairment and that nephrotoxicity is often detected only when serum creatinine rises on routine labs, underscoring the need for regular renal function monitoring in patients treated with 5-ASA.
- Mesalazine-associated interstitial nephritis – (Nephrology Dialysis Transplantation): A classic paper reviewing cases of mesalazine-associated interstitial nephritis found that renal impairment of any severity may occur in up to 1 in 100 patients, while clinically significant interstitial nephritis occurs in fewer than 1 in 500 patients. When diagnosis of nephrotoxicity was delayed for 18 months or more after treatment began, restoration of kidney function after drug withdrawal did not occur, leaving many patients with permanent loss of function.
- Retrospective cohort of 151 patients with 5-ASA nephrotoxicity (Heap et al.): A retrospective study of 151 patients with inflammatory bowel disease and definite or probable 5-ASA–associated nephrotoxicity reported that only about 30% fully recovered kidney function after stopping the drug, while nearly 10% required renal replacement therapy (dialysis or transplant). Longer duration of 5-ASA therapy and higher average dose were associated with more severe and permanent renal damage, illustrating how prolonged exposure worsens outcomes.
- Pediatric case review – mesalazine-induced kidney injury (Frontiers in Pediatrics): A pediatric case report and literature review on mesalazine-induced kidney injury in children with inflammatory bowel disease found that kidney injury often presents with abnormal urinalysis and can progress to end-stage renal disease in a subset of cases. The authors emphasize that renal function should be monitored regularly in pediatric patients receiving mesalamine and note that at least 10% of patients with mesalamine-induced interstitial nephritis progress to end-stage renal disease.
- Mesalamine-induced chronic tubulo-interstitial nephritis (review): A review of mesalazine-induced interstitial nephritis reported that, although overall nephrotoxicity in 5-ASA-treated patients is rare, about 61% of affected individuals are left with residual chronic renal insufficiency and approximately 13% develop end-stage renal disease. The authors describe most cases as idiosyncratic, not strictly dose-dependent, and often detected late because symptoms are nonspecific or absent.
- Kidney stones and mesalamine nephrolithiasis: Pharmacovigilance reports and a case series describe kidney stones composed of mesalamine in patients treated with the drug, as well as radiolucent mesalamine stones that can be missed on standard imaging. These reports identify mesalamine-related kidney stones as an additional form of renal involvement, particularly in patients with long-term or high-dose exposure.
Types of Kidney Injury Linked to Asacol/Mesalamine
Asacol and other mesalamine products are associated with several forms of kidney injury that can develop gradually and silently in patients who rely on these medications for long-term management of inflammatory bowel disease.
Medical literature shows that many individuals experience renal complications only after prolonged exposure, especially when their doctors do not perform routine bloodwork to track serum creatinine or declining kidney function.
The drug’s toxicity most often appears as inflammation in the kidney’s tubulointerstitial compartment, but additional patterns of injury have been documented in both adult and pediatric patients.
Some patients develop sudden renal symptoms, while others learn of kidney damage only when testing reveals advanced impairment.
Once these injuries progress, especially in the absence of consistent monitoring, the resulting kidney disease can become permanent.
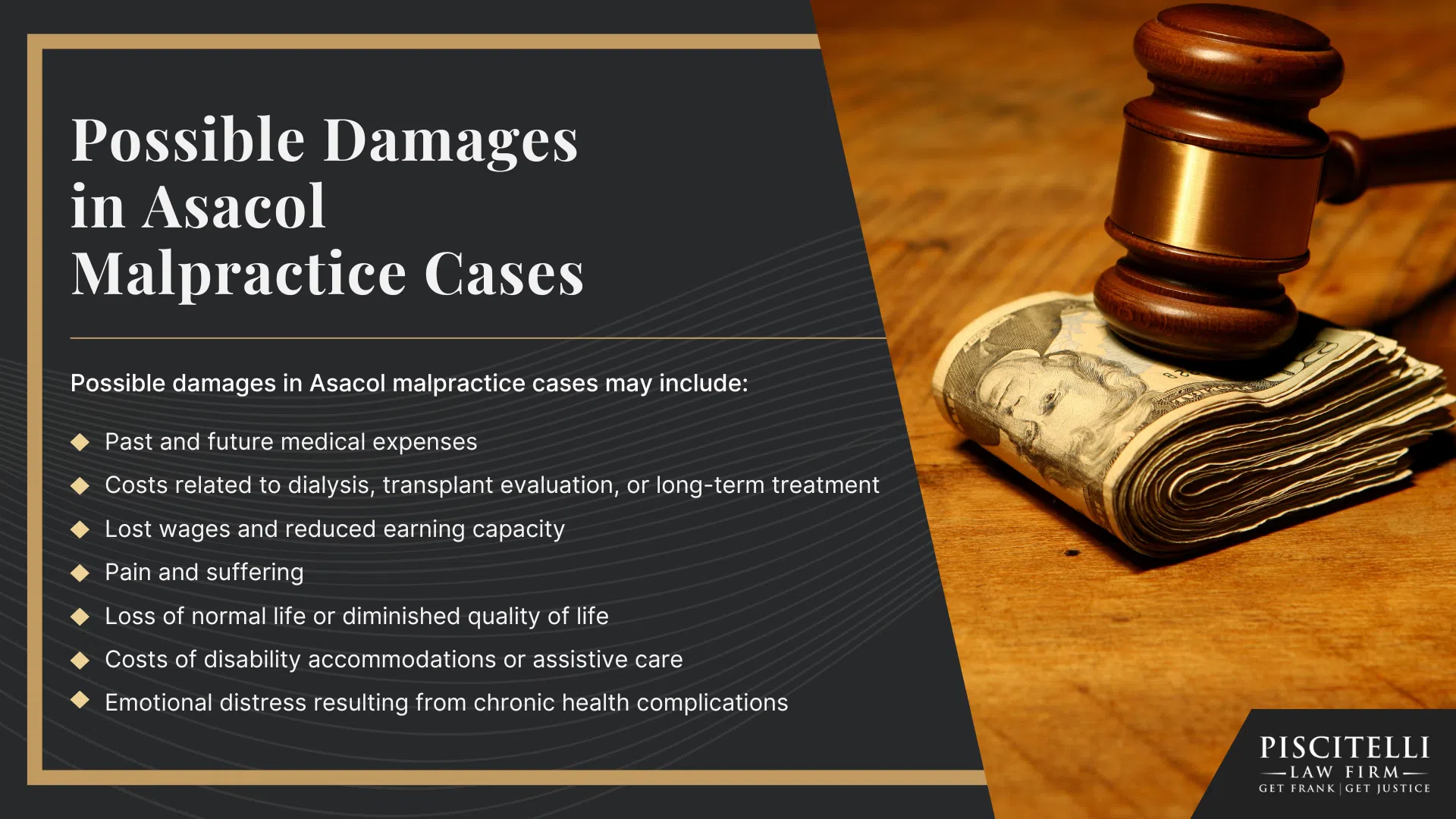
A subset of patients ultimately experience kidney failure requiring dialysis or transplant.
Types of kidney injury reported in association with Asacol/mesalamine include:
- Acute interstitial nephritis (AIN)
- Chronic interstitial nephritis (CIN)
- Chronic tubulointerstitial nephritis (CTN)
- Minimal change disease / nephrotic syndrome
- Acute kidney injury (AKI) and chronic kidney disease (CKD)
- Progression to end-stage renal disease (ESRD)
- Kidney stones related to mesalamine exposure
Onset, Subtle Presentation, and Why Doctors are Supposed to Monitor Renal Function
Kidney injury associated with Asacol often develops slowly, which makes early detection difficult without appropriate monitoring.
Adult patients taking mesalamine may feel generally well even as their kidney function declines, because early renal impairment rarely produces noticeable symptoms.
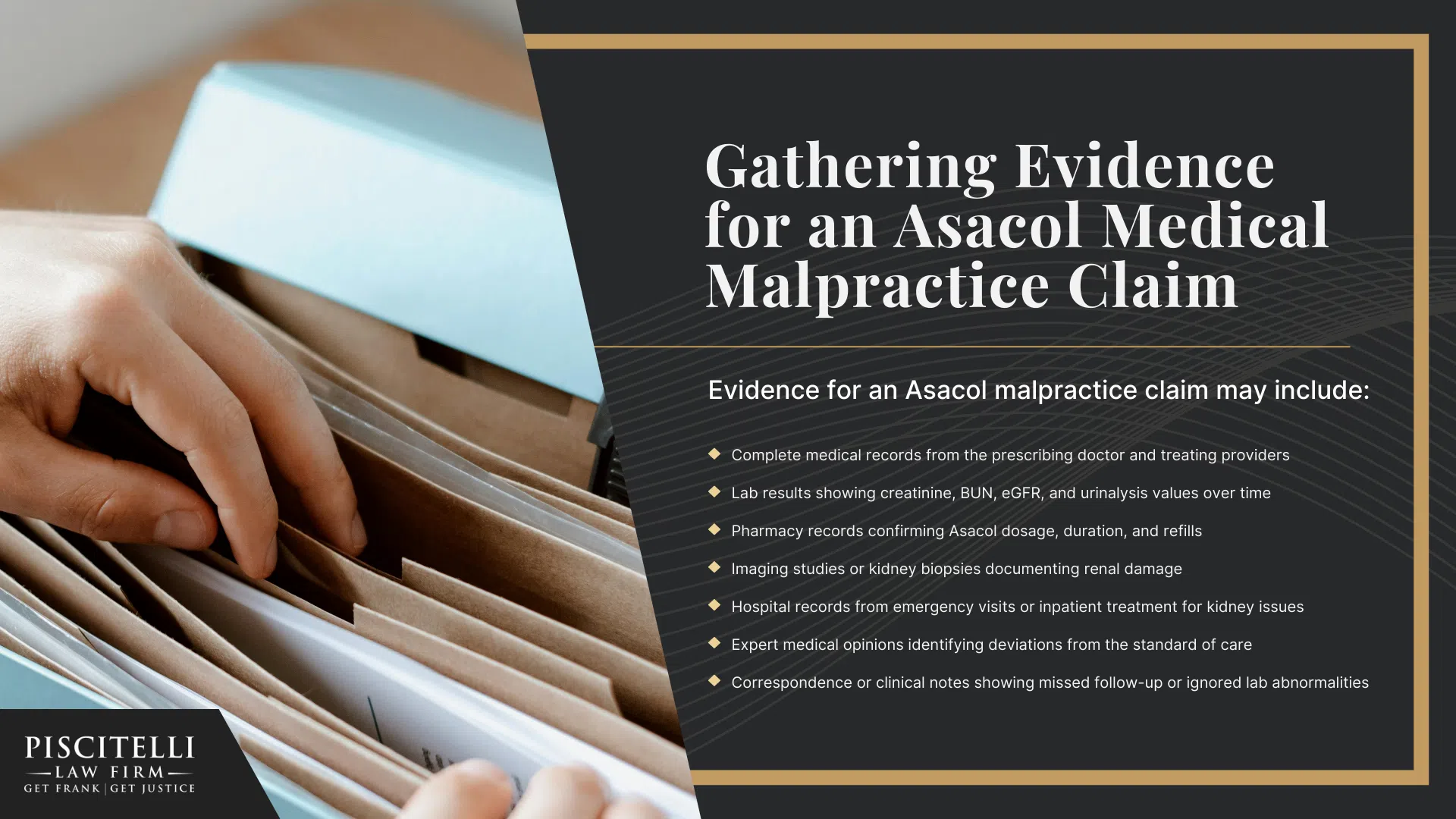
Many cases are identified only after routine bloodwork shows elevated creatinine or reduced glomerular filtration rates, and in some instances, kidney biopsies performed later reveal advanced inflammation that had been progressing quietly for months or years.
This pattern contributes to situations where mesalamine toxicity is recognized too late, allowing reversible injury to evolve into chronic damage that rarely returns to baseline.
Because renal failure is rarely immediate and early warning signs are subtle or absent, the burden falls on physicians to order baseline tests, perform scheduled lab monitoring, and respond quickly to any signs of decline.
When doctors fail to monitor renal function as expected, patients lose the opportunity for early intervention and face permanent kidney complications that could have been prevented with proper oversight.